In November, George Mason University launched the first and only College of Public Health (CPH) in the Commonwealth of Virginia to meet the critical growing need for skilled, interdisciplinary health professionals and research across the state.

“Mason’s College of Public Health graduates will bring new and diverse talent to Virginia’s health workforce, addressing critical shortages and building a strong talent pipeline for the long-term health of the region,” says Mason President Gregory Washington. “Individuals, families, and communities will benefit from discoveries, clinical care, and public health practice initiatives generated by this multidisciplinary college.”
With CPH, Virginia becomes the 36th state in the country to have a college dedicated to public health and will benefit from increased community engagement, workforce development initiatives, and research of consequence with a focus on eliminating health disparities.
The college enrolls more than 1,900 undergraduate and 1,300 graduate students in nationally recognized programs, including six undergraduate degrees, eight master’s degrees, five doctoral degrees, and six professional certificate programs. The college includes the School of Nursing and the departments of Global and Community Health, Health Administration and Policy, Nutrition and Food Studies, and Social Work.
AN INCLUSIVE APPROACH
Public health and health care fields are striving to better reflect and serve the nation’s diverse communities. At Mason, we believe inclusivity is our strength. To meet the region’s and the commonwealth’s needs, Mason’s College of Public Health is focused on an inclusive approach to public health education, research, and practice. Of the college’s more than 3,200 students, 60 percent are from historically underrepresented groups and 32.5 percent of its undergraduates are first-generation college students.
Mason’s proximity to Washington, D.C., and the federal health-related agencies, leading health systems, policy-making institutions, nonprofit community service organizations, and global health consulting management firms located here in Northern Virginia make it an ideal hub for researching, teaching, influencing, and improving public health and well-being.
With more than 500 partners, including Inova Health System and Sunrise Senior Living, the college is well positioned to address the full spectrum of factors that influence the public’s health and well-being throughout an individual’s lifespan.
THE INTERPROFESSIONAL ADVANTAGE
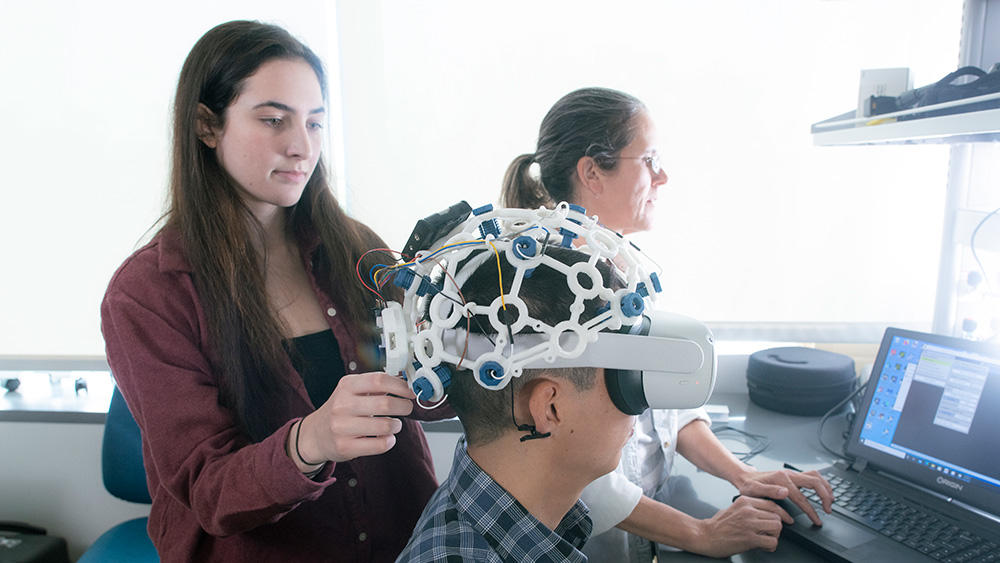
The college’s distinct combination of departments allows Mason to see public health differently and creates an interprofessional advantage for learning, research, and practice. Its interprofessional research and experiential learning fosters knowledge-sharing to improve outcomes.
CPH prepares professionals committed to delivering inclusive health and well-being through competency- based curriculum and national workforce growth initiatives. The majority of its students graduate with inter-professional research, clinical, practicum, or capstone experience that sets them apart.
“As the first and only College of Public Health in Virginia, this launch reflects our academic and research mission and the pivotal leadership role we play in population health and well-being,” says Dean Melissa J. Perry, who joined Mason in August. “Our distinctive set of degree offerings, our inclusive approach to research and education, and our commitment to experiential learning opportunities prepare students to thrive in multicultural environments.”
Here are some of the ways Mason and the college are working to make a difference in Virginia.
TEACHING AND LEARNING
Experiential learning and hands-on training are the hallmarks of a Mason education and imperative to preparing graduates to be career-ready. Through internships, practicums, research experiences, study abroad, or clinical practice, students train for their intended field and leave Mason with the confidence and skills to make

A difference in the health of people and populations. CPH delivers these experiences to students in a variety of ways while bettering public health, as detailed below and on the following page.
Interprofessional behavioral health clinic provides real-world experience: To combat the lack of affordable mental health services, Mason opened a first-of-its-kind interprofessional clinic where psychiatric mental health nurse practitioner students and clinical psychology doctoral students deliver services in collaboration with licensed faculty. It is the only clinic in the country for affordable psychiatric medication management services that also serves as an experiential learning environment for students.
Nutrition clinic provides hands-on dietitian training: In the new nutrition clinic at Mason’s Population Health Center, students have an additional source of hands-on learning. The sliding scale clinic trains graduate students in nutrition under the direct supervision of faculty who are registered dietitians or MDs.
Students gain global perspective on HIV/AIDS health care: College of Public Health students traveled to Amsterdam in 2022 to study how policies and access to care affect those with HIV/AIDS. From a global public health perspective, students learned about reducing stigmas associated with sexually transmitted infections, as well as how sexual health policy and culture in Amsterdam compare to the United States.
RESEARCH AND INNOVATION
Improving forensic bruise analysis: School of Nursing professor and forensic nurse Katherine Scafide has long served people who’ve experienced violence. In her research, Scafide is using alternate light sources technology to help identify hard-to-see bruising in a variety of skin tones. A $1 million grant from the U.S. Department of Justice will help pair Scafide’s forensic bruise analysis with machine learning to improve documentation. She is working with Janusz Wojtusiak, director of Mason’s Machine Learning and Inference Laboratory, and engineering professor David Lattanzi on the project.
Preventing suicide among essential workers: A strong healthcare system isn’t just based on the health of its patients but is equally committed to its essential healthcare workers. CPH’s Farrokh Alemi and a team of researchers are studying how gender, racial/ethnic, medical history, and socioeconomic status affect suicide patterns among essential workers and whether COVID-19 contributes to suicide beyond these factors. The study, supported by the Gates Foundation, Healthcare Cost Institute, and Cornell University, aims to provide evidence-based policy recommendations and a public health framework with targeted mitigation strategies, medical interventions, and other recommendations to reduce sociodemographic disparities in suicide for patients, essential workers, and health care systems.
Improving access to care through telehealth: Mason researchers Alison Cuellar and Leah Adams, MA Psychology ’10, PhD ’14, received a grant from the National Institute for Health Care Management Foundation to study health equity and the impact of Medicaid’s telehealth policy. The findings are expected to inform federal and state policymakers as they consider whether and how to extend telehealth policies and to identify remaining policy gaps—particularly among marginalized communities.
WORKFORCE DEVELOPMENT
When organizations like the U.S. Health Resources and Services Administration (HRSA) and AmeriCorps tackle critical health care workforce shortages, they turn to Mason. In 2022, the college received several $1 million+ grants to deliver major workforce initiatives.
Building the behavioral health workforce and improving access: The $1.9 million HRSA Behavioral Health Workforce and Training grant is helping improve access to behavioral health services for underserved and rural populations through the Mason Community–Academic Partnerships in Behavioral Health program, led by the Department of Social Work. The program provides yearly stipends for master of social work students and expands the existing partnership with the Mason and Partners (MAP) Clinics. Professor Denise Hines codirects the project with Social Work chair Emily Ihara.
Preparing nurses to care for underserved populations: A $1.15 million HRSA grant helped create an interprofessional Learning Laboratory for Community Health that prepares students to work in medically underserved communities in inner cities and rural areas and with under-served populations such as aging adults and patients of color. Students design and implement evidence-based solutions and examine population health solutions for communities. School of Nursing professor Rebecca Sutter, MSN ’01, DNP ’12, leads the program.
Building workforce resiliency and well-being: A three-year $2 million cooperative agreement with HRSA supports the mental health and well-being of current and future health care workers through in-person and virtual education and training activities. The program supports nurses, social workers, public health professionals, and practitioners in rural and underserved communities. Professor Debora Goldberg leads the program.
Training public health workers to better connect patients with care: Funded through a $2.6 million grant from the Public Health AmeriCorps program, the Mason Data and Technology Driven Public Health AmeriCorps Training Program will improve patient referrals for both health and social determinants of health needs using data analytics and community-based relationships. Sutter and Wojtusiak, director of the Center for Discovery Science and Health Informatics, lead the program.
Addressing the critical nursing shortage in the region: The School of Nursing and MedStar Washington Hospital Center have partnered to create the Future Nurse Program, which prepares nurses for clinical practice. MedStar Health will cover in-state tuition for Future Nurse Program students in Mason’s Accelerated Second Degree BSN Program who agree to work for three years as full-time licensed registered nurses at MedStar Washington Hospital Center after graduation.
COMMUNITY OUTREACH
The name College of Public Health more accurately reflects the pivotal role CPH plays in the health and well-being of the community and the region. The Population Health Center houses state-of-the art facilities for telehealth, research, and delivering clinical care. Operated by Mason’s School of Nursing, MAP Clinics serve the underinsured and uninsured communities in Prince William and Fairfax Counties by providing low-barrier access to acute and chronic health care services, school physicals and childhood immunizations, screenings, and mental health services for vulnerable populations.
Innovating to meet the need of the community: MAP Clinics received the Innovative Practice or Partnership of the Year award as part of the Prince William County Chamber of Commerce 2022 Business Awards for its trailblazing work with the City of Manassas Park Public Health Department and Prince William County Health Department.
Using social media to promote hepatitis B screening among Korean Americans: Asian Americans, who make up only 7 percent of the U.S. population, make up 50 percent of all hepatitis B (HBV) cases. Foreign-born Asian Americans face many barriers to HBV screening, vaccination, and treatment because of lack of HBV-related knowledge, stigma, and limited access to health care due to language barriers and immigrant status. To address this public health need, a team of interdisciplinary Mason researchers, led by Professor Alicia Hong and the Korean American Outreach Group, developed “Let’s talk about liver cancer,” the first social media-based liver cancer prevention program specifically for Korean Americans.
New initiative promotes healthy aging and professional development: The college and ServiceSource Inc. have established the Northern Virginia Center on Aging, which will provide services, programs, and activities for older adults and workforce development and continuing education for the health care professionals who support them. Mason students will have access to practicums, internships, and other experiential learning opportunities on how to effectively work with older adults. The center is a recognized satellite center for the statewide Virginia Center on Aging.
Using personalized nutrition to help prevent type 2 diabetes: Professor Raedeh Basiri’s new clinical trial seeks to answer whether personalized nutrition intervention can be effective in lowering blood sugar in people with prediabetes, thereby helping to prevent or delay type 2 diabetes and related cardiovascular diseases.
Mary Cunningham, John Hollis, Michelle Thompson, and Preston Williams contributed to this article.
Topics

More from CPH
- February 2, 2026
- January 30, 2026
- January 27, 2026
- January 26, 2026
- January 21, 2026
