In This Story
Healthy individuals can often take simple movements for granted, but after a neurological event such as a stroke or traumatic brain injury, simple motions like grasping an object or flexing an ankle can become quite difficult and even frustrating.
George Mason University Assistant Professor Quentin Sanders and his team of researchers at the ImPoWer Lab in the College of Engineering and Computing are finding ways to make these activities easier by inventing and improving rehabilitative and assistive technologies.
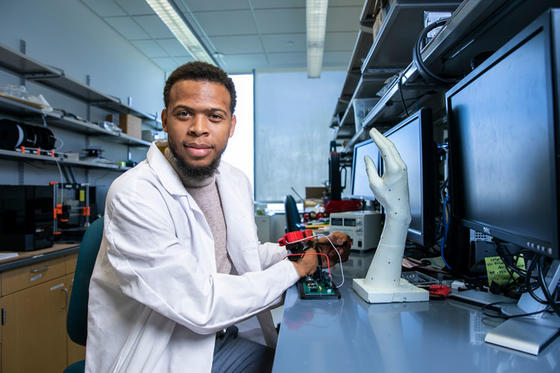
Photo by Ron Aira / Creative Services / George Mason University
The lab’s research team seeks to develop innovative and globally relevant rehabilitation, robotic, and prosthetic devices to enhance the quality of life of individuals who have experienced a neurological injury or amputation. But more than that, Sanders hopes to empower researchers and students to see themselves as scientists and scholars.
Two new members of the team have promising ideas. The first is post-doctoral researcher Nelson Glover who earned his PhD from The Ohio State University in 2022. Glover is funded by the eFellows Post-doctoral Fellowship, sponsored by the American Society for Engineering Education and the National Science Foundation. He seeks to develop wearable, portable, and economical solutions for gait retraining for people who have experienced neurological injuries.
According to Sanders, most current solutions require bulky and expensive equipment, but Glover has a different idea. Glover’s device uses small, inexpensive sensors to measure the muscle movements and forces of the ankle.
He says, “This type of training is called biofeedback. Usually, you're giving a person feedback based on some type of biological signal that you're measuring to induce some type of behavioral change. In our approach, we are providing people feedback based on forces that we're measuring with these sensors and seeing if they can alter ankle propulsion forces.”
Sanders’ second new team member is PhD student, Mohammad Shams who is developing a standardized framework for evaluating rehabilitative devices outside the clinical setting.
The study begins with a very, very large data set from a thousand users who use a device that Sanders’ previous PhD advisor created. The device, a wearable sensor, is one that people use for hand therapy.
Sanders says, “What's nice about this large data set is that we can start to get a sense of how they're adapting different parameters when they're in the wild when they're not in the clinic when the therapist isn't there. We can find out why they aren’t using this device, or what they like about the device.”
Sanders compares it to the kind of user reports that makers of smartphones use all the time. Companies use them to improve features and functions and make them more appealing to consumers. He says, “We don't have that for a lot of devices. So, a lot of times you'll try a device on in this very controlled setting but it often isn’t very realistic.”
The research aims to leverage Artificial Intelligence and machine learning to develop algorithms in this project as well. For example, if you see, someone trending towards abandoning the use of the technology, the researchers could program an algorithm that sends a reminder and tells the user to try something different.
“I really like this project a lot, it's answering a lot of fundamental questions about rehabilitation device usage that we don't really have the answers to yet,” says Sanders.
